Life expectancy in Britain has fallen so much that a million years of life could disappear by 2058 – why?
Courtesy of Danny Dorling, University of Oxford and Stuart Gietel-Basten, Hong Kong University of Science and Technology

via shutterstock.com
Buried deep in a note towards the end of a recent bulletin published by the British government’s statistical agency was a startling revelation. On average, people in the UK are now projected to live shorter lives than previously thought.
In their projections, published in October 2017, statisticians at the Office for National Statistics (ONS) estimated that by 2041, life expectancy for women would be 86.2 years and 83.4 years for men. In both cases, that’s almost a whole year less than had been projected just two years earlier. And the statisticians said life expectancy would only continue to creep upwards in future.
As a result, and looking further ahead, a further one million earlier deaths are now projected to happen across the UK in the next 40 years by 2058. This number was not highlighted in the report. But it jumped out at us when we analysed the tables of projections published alongside it.
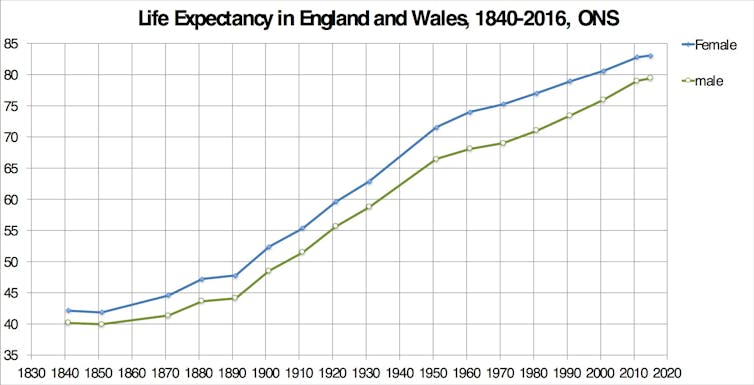
It means that the 110 years of steadily improving life expectancy in the UK are now officially over. The implications for this are huge and the reasons the statistics were revised is a tragedy on an enormous scale.
A rising tide of life
Life expectancy is most commonly calculated from birth. It is the average number of years a new-born baby can expect to live if the mortality rates pertaining at the time of their birth apply throughout their life.
In 1891, life expectancy for women in England and Wales was 48 years. For men it was 44. Many people lived longer than this, but so many babies died in their first year of life that, from birth, you were doing better than average if you made it past your forties. For most of the 1890s the Conservatives were in power under Lord Salisbury. They continued to support and build on public health reforms from earlier years, such as the construction of sewers and improvements to the supply of clean piped water. Often these reforms were instigated by local government, which was able to be more proactive than it is today. Adult health improved and by 1901, on average, women lived to 52 and men 48.
The turn of the century saw the start of dramatic improvements in infant mortality as everyday sanitation became paramount and the condition and living standards of mothers started being taken more seriously. The Liberal prime ministers Henry Campbell-Bannerman, Herbert Henry Asquith and David Lloyd George were in charge as most of these improvements occurred. These ranged from the recognition and widespread acceptance that germs cause disease though to the provision of better insurance and pensions, paid for by more progressive taxation. By 1921, women lived to 60 and men to 56.
Life expectancy continued to soar ahead. By 1951, 30 years later, women lived to 72 and men to 66. It rose by more than a year every three years at this time, despite World War II, rationing and 1940s and 1950s austerity. Back then we really were all in it together. For women, better maternity care and the fact that most did not smoke had given them the edge.
National Life Tables: England and Wales 2014-2016 and 1840-2011. Office for National Statistics, Author provided
Improvements in life expectancy slowed in the 1950s under the Conservative government of Harold Macmillan. To be fair, most of the easy early wins had been achieved, such as clean water supplies and free access to health care at the point of delivery with the introduction of the NHS in 1948. Still, Macmillan tried to pretend that deaths from smog in London were due to influenza. The Conservatives were never able to achieve anything as impressive for public health as Labour’s launch of the NHS, which had an immediate effect simply by boosting national morale and access to care, and on infant health. Despite that, and with some help from the policies of Harold Wilson’s first Labour government in the 1960s, by 1971 women lived to 75 and men to 69. This improvement was driven by more spending on health services, including the widespread introduction of incubators for new-born babies that needed them, as well as improvements in housing conditions.
In the 1970s, the rate of improvement in life expectancy across England and Wales accelerated again. To be young in those days was to feel progress all around you. People back then lived longer in the city of Sheffield than the national average and, for a few years in the 1970s, the population centre of the country moved northwards. Social progress in the 1970s meant that despite the terrible cutbacks in healthcare funding in the 1980s under Margaret Thatcher’s Conservative government, by 1991 women were living to 79 years and men to 73. The long-term effects of more people stopping smoking in earlier decades had begun to have a particularly significant effect.
The next two decades, under the premierships of John Major, Tony Blair and Gordon Brown, would see men catch up with women a little. This was because in the 1990s there were still many male smokers who could give up smoking. For women, the effect was less dramatic because fewer women had smoked to start off with. By 2011, women in England and Wales were living to 83 years and men to 79 years.
Flatlining
And then, after 2011, under the Conservative-led governments of David Cameron and Theresa May, nothing. No improvement. Life expectancy flat-lined.
The latest figures for the period 2014 to 2016 were published in September 2017. Women can now expect to live to 83.06 and men to 79.40. For the first time in over a century, the health of people in England and Wales has stopped improving.
Just as Macmillan had done before in the 1950s, the 2010 coalition government initially tried to blame influenza. But as the years passed and life expectancy continued to stall, it became clear that it wasn’t because of flu or an illness like it. The most plausible culprit was a combination of the particular kind of austerity for the poor and elderly that the 2010 Conservative-Liberal Democrat government so quickly enacted.
This led to the loss of care support to half a million elderly people by 2013. NHS budgets stalled or fell slightly in the years following 2010-11 and many old-age care homes went bankrupt. There was a rise in fuel-poverty among the old. Sanctions and cuts to disability benefits were introduced, alongside many more aspects of increased economic callousness.
Those first affected were elderly women in the poorest parts of the UK. They lived in geographical areas that had been targeted by the previous Labour government for policy interventions to improve health. All those schemes stopped after 2010. Attempts throughout 2014 and 2015 to point out that the people’s health was deteriorating were either ignored or even rebutted by those who had been appointed by the 2010 government to safeguard the nation’s health.
By 2016, cuts in welfare spending, especially to older pensioners had been linked to a rise in deaths – initially among elderly women and later older people in general living in poorer areas. Public health experts writing in the British Medical Journal called for an inquiry, but none came. Instead, the government’s public health officials continued to claim that: “Recent high death rates in older people are not exceptional.”
The situation in Scotland was even worse than that in England and Wales, but again there was no official response when this was pointed out. In hindsight, there was wilful neglect by politicians, tinged by officials’ fear of upsetting their political masters in a time of savage spending cuts.
At first almost everyone kept quiet, but eventually it became too stark a situation to ignore. By summer 2017, Michael Marmot’s Institute of Health Equity was linking health services cuts to the rise in dementia deaths and the faltering national life expectancy. Researchers at Liverpool, Oxford, Glasgow and York universities connected some of the stalling in health improvements to delays in discharging patients from hospital due to insufficient older adult social care. Earlier in the year, the Financial Times reported that the deceleration of previous rises in life expectancy was so rapid that it had cut £310 billion from future British pension fund liabilities. And this was just for a few of the larger pension schemes.
On November 16, an article in the British Medical Journal Open concluded that severe public spending cuts in the UK were associated with 120,000 deaths between 2010 and 2017. Just over a third of these occurred between 2012 and 2014 and almost none in 2010 or 2011. The rate of death due to austerity was rising and there was what is called a “dose-response relationship” between cuts and rising mortality. This term, commonly used as part of the evidence needed to establish that a medicine is beneficial, means that as you increase the dose of an intervention the responses to it rise at the same rate. It can also be used to indicate likely causes of harm.
In this case it indicated that the more cuts there have been to public health, social services and benefits – particularly for people in old age – the more earlier deaths there have been in the UK. Cuts that prevent visits by social workers to elderly people reduce their chances of being found after a fall at home. Cuts that make it harder to rehouse someone who is currently in a hospital bed back into the community, result in hospital beds not being available for others.
Very recently, the economist Simon Wren-Lewis also looked into the link between austerity and mortality and explained:
It is one thing for economists like me to say that austerity has cost each household at least £4,000: this can be dismissed with ‘what do economists know’? But when doctors say the policy has led to premature deaths, that is something else.
Life expectancy for women in the UK is now lower than in Austria, Belgium, Cyprus, Finland, France, Germany, Greece, Iceland, Ireland, Italy, Liechtenstein, Luxembourg, Malta, The Netherlands, Norway, Portugal, Slovenia, Spain and Sweden. Often it is much lower. Men do little better, as the graph below shows.
The UK’s lowly position in the European league table mean that the stalling in life expectancy improvements has nothing to do with a limit being reached. As yet, nowhere has reached a limit, and many countries are now far ahead of the UK.
In almost all other of the most affluent countries, apart from the US, people live longer lives than in the UK, often many years longer, and the best countries continue to pull away – leaving the UK and US even further behind.
What matters most is what happens next.
A million lives lost
The stagnation in life expectancy is no longer being treated as a “blip”. It is now projected to be the new norm. But the ONS does not explicitly state this in its projections for the future. To calculate the figure of a million lives lost you have to subtract all the future deaths now predicted in the 2017 report, which was based on data from 2016, from those projected two years ago, based on a 2014 projection.
Every year up until at least the year 2084, people across the UK are now expected to die earlier. Already in the 12 months between July 2016 and June 2017, we calculated that an additional 39,307 more people have died than were expected to die under the previous projections. Over a third, or 13,440, of those additional deaths have been of women aged 80 or more who are now dying earlier than was expected. But 7% of these extra deaths in 2016-17 were of people aged between 20 and 60: almost 2,000 more younger men and 1,000 more younger women in this age group have died than would have if progress had not stalled. So whatever is happening is affecting young people too.
The projection that there will be a million extra deaths by 2058 is not due to the fact that there will simply be more people living in the UK in the future. By contrast, the ONS now projects less inward migration. The million extra early deaths are not due to more expected births: the ONS now projects lower birth rates. The extra million early deaths are simply the result of mortality rates either having risen or having stalled in recent years. The ONS now considers that this will have a serious impact on life expectancy in the UK and population numbers for decades to come.
If you are in your forties or fifties and live in the UK this is mostly about you. Almost all of the million people now projected to die earlier than before – well over four-fifths of them – will be people who are currently in this age group: 411,000 women and 404,000 men aged between 40 and 60. Child, infant mortality and still births have also not improved recently – and again this has recently been linked to under-funding resulting in under-staffing in the NHS.
It easy to dismiss these statistics with remarks such as: “people live too long nowadays anyway” and: “I wouldn’t want to live that long”. But older people are important and grandparents are often a formative part of a child’s life. Because many people in the UK are now having children at older ages, this will translate into more people not seeing their grandchildren grow up. But, above that, longer, healthier lives have been the most important marker of social progress in Britain for well over a century. And now, for the first time in a century, we are no longer expected to see the rates of improvement we have become used to.
Projections are not predictions
Population estimates are always hard to make and even harder to explain. In 1990, in the New York Review of Books, the economist Amartya Sen wrote that: “More than 100m women are missing” in the world. Sen wrote that compared to men in Europe and North America:
The fate of women is quite different in most of Asia and North Africa. In these places the failure to give women medical care similar to what men get and to provide them with comparable food and social services results in fewer women surviving than would be the case if they had equal care.
There is some irony that a quarter of a century later we now have to ask why, in one of the richest countries of the world, are we now not expecting people to enjoy as long a life as we were expecting them to just two years ago?
The government accepts that air pollution already contributes to around 40,000 premature deaths a year. Why then is there not more public outrage when an additional 39,307 deaths occurred in the year up until June 2017 than had been expected? And it happened the year after an additional 30,000 people had already died in 2015.
In November 2017, the ONS went on to project that there will be more than an extra 25,000 deaths between July 2017 and June 2018. Then an extra 27,000 deaths in the 12 months after that, more than an extra 28,000 deaths the year after that – and on and on and on. It now looks as if we should come to expect heightened mortality year after year until the end of our lives.
The government has given no reason for why this is happening. But there is absolutely no reason to suppose that this is due to something beyond our control.
Whatever has happened it is not a sudden worsening of the healthy behaviour of people in the UK. It is not a sudden rise in obesity or some additional carelessness about looking after ourselves. Neither obesity nor any other human behaviour linked to poor health such as smoking or drinking alcohol has seen a sudden rise. In fact, health complaints from smoking have plummeted since the introduction of the 2007 ban on smoking in public places. The number of Britons who smoke is at its lowest level.
The proportion of adults who drink alcohol in the UK is also currently at its lowest level since 2005. Obesity is still rising, but it has been for decades now, and the age groups now dying in high numbers – the over 80s – are not yet those who became obese in recent decades.
The most likely culprit, by far, is austerity, including the effect of the cuts to social and health care services.
We will not live longer by all taking responsibility just for ourselves alone, looking after just us and our families, trying to get fitter, eat better and worry less. This is not how the health of whole nations improves. It is about all of us, not just one of us. That is why it is a million years of life. And we should not allow that million to be announced quietly, like the inevitable dying of the light.
As we argue in our new book, demography is not destiny. Projections are not predictions. There is no preordained inevitability that a million years of life need be lost, but already, 120,000 have been by 2017.
![]() The rest of those million early deaths could be avoided. There is no biological reason why life expectancy should be so low in the UK compared to almost all other affluent nations. The social sciences and epidemiologists between them have the answers, but only through politics comes the power to make the changes that are now so urgently needed.
The rest of those million early deaths could be avoided. There is no biological reason why life expectancy should be so low in the UK compared to almost all other affluent nations. The social sciences and epidemiologists between them have the answers, but only through politics comes the power to make the changes that are now so urgently needed.
Danny Dorling, Halford Mackinder Professor of Geography, University of Oxford and Stuart Gietel-Basten, Associate Professor of Social Science and Public Policy, Hong Kong University of Science and Technology
This article was originally published on The Conversation. Read the original article.