Reminder: Pharmboy and Ilene are available to chat with Members, comments are found below each post.
How Alzheimer's disease spreads throughout the brain – new study
Courtesy of Thomas E Cope, University of Cambridge
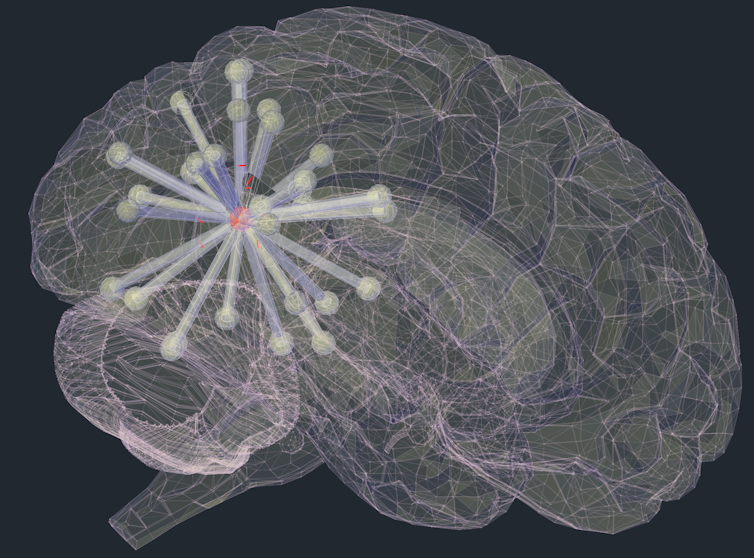
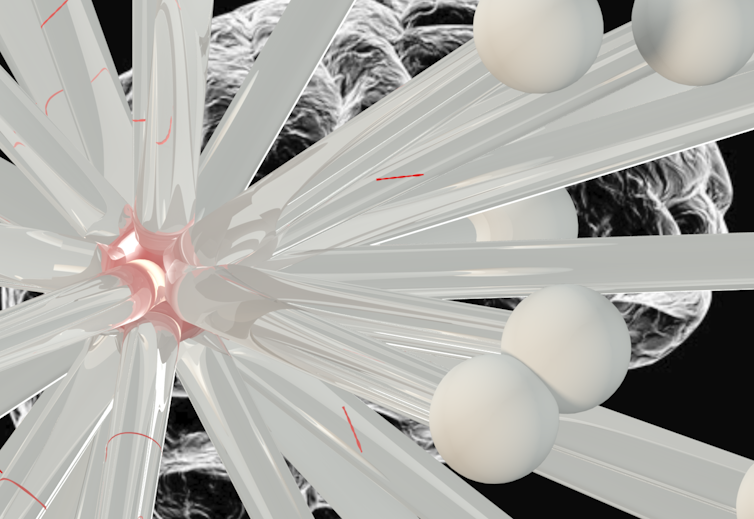
Harmful tau protein spreads through networks. Author provided
Alzheimer’s disease is a devastating brain illness that affects an estimated 47m people worldwide. It is the most common cause of dementia in the Western world. Despite this, there are currently no treatments that are effective in curing Alzheimer’s disease or preventing its relentless progression.
Alzheimer’s disease is caused by the build-up of two abnormal proteins, beta-amyloid and tau. Tau is particularly important because it causes neurons and their connections to die, preventing brain regions from communicating with each other normally. In the majority of cases, tau pathology first appears in the memory centres of the brain, known as the entorhinal cortex and hippocampal formation. This has been shown to occur many years before patients have any symptoms of disease.
Over time, tau begins to appear in increasing quantities throughout the brain. This causes the characteristic progression of symptoms in Alzheimer’s diseases, where initial memory loss is followed by more widespread changes in thinking and behaviour that lead to a loss of independence. How this occurs has been controversial.
Transneuronal spread
In our study, published in Brain, we provide the first evidence from humans that tau spreads between connected neurons. This is an important step, because stopping this spread at an early stage might prevent or freeze the symptoms of Alzheimer’s disease.
This idea, called “transneuronal spread”, has been proposed before and is supported by studies in mice. If abnormal tau is injected into a healthy mouse brain, it quickly spreads and causes the mice to manifest dementia symptoms. However, it had not previously been shown that this same process occurs in humans. The evidence from mouse studies was controversial, as the amount of tau injected was relatively high, and disease progression occurred much more rapidly than it does in humans.
Artist’s impression of tau spreading between connected neurons. Author provided
In our study, we combined two advanced brain imaging techniques. The first, positron emission tomography (PET), allows us to scan the brain for the presence of specific molecules. With this, we were able to directly observe the abnormal tau in living patients, to see exactly how much of it was present in each part of the brain.
The second, functional magnetic resonance imaging (fMRI), measures blood flow in the brain in real time. This allowed us to observe the activity produced by brain regions communicating with each other. For the first time, by scanning the same people with both methods, we were able to directly relate the connections of the brain to the distribution of abnormal tau in living humans with Alzheimer’s disease.
We used a mathematical technique called “graph analysis” to analyse brain connectivity. This technique involved splitting the brain up into 598 regions of equal size. We then treated the connectivity between regions like a social network, assessing factors such as the number of contacts a brain region had, how many “friendship” groups it took part in, and how many of a brain region’s contacts were also contacts of each other.
In a flu epidemic, people with a large number of social contacts are most likely to become infected and then to pass the infection on to others. Similarly, the transneuronal spread hypothesis predicts that strongly connected brain regions will accrue most tau. This is what we observed. This relationship was present within each brain network individually, as well as across the whole brain.
We were also able to exclude potential alternative explanations for the appearance of tau throughout the brain. It had previously been suggested that tau might appear at brain regions that were vulnerable because of high metabolic demand or a lack of support from their neighbours. While it is possible that these factors are important in neuronal death, our observations were not consistent with them being the primary drivers of the initial accumulation of abnormal tau.
In addition, by looking at patients with a range of disease severity, from mild cognitive impairment through to established Alzheimer’s disease, we were able to disentangle the causes of tau accumulation from its consequences. We showed that increasing amounts of tau in Alzheimer’s disease caused the brain to become less connected overall, and the connections that remained became increasingly random.
Long-range connections
Finally, we contrasted the findings in Alzheimer’s disease to a rarer condition called progressive supranuclear palsy (PSP), which affects approximately three in every 100,000 people. This condition is also caused by tau, but it remains confined to the base of the brain. We demonstrated that in PSP the evidence did not support transneuronal spread. This might be because of the different structure of abnormal tau pathology in the two diseases. In Alzheimer’s disease, tau is present in “paired helical filaments”, while in PSP it is in “straight filaments”.
Damaged communications. Shutterstock
We showed that as PSP progresses, direct long-range connections are preferentially damaged, meaning that information had to take a more indirect route across the brain. This might explain why, when asked a question, patients with PSP usually respond slowly but correctly.
![]() Overall, evidence of transneuronal spread in humans with Alzheimer’s disease provides proof of concept for exciting new treatment strategies to lock up tau pathology before it can cause significant damage.
Overall, evidence of transneuronal spread in humans with Alzheimer’s disease provides proof of concept for exciting new treatment strategies to lock up tau pathology before it can cause significant damage.
Thomas E Cope, Academic Clinical Fellow, University of Cambridge
This article was originally published on The Conversation. Read the original article.