Reminder: Pharmboy is available to chat with Members, comments are found below each post.
Diabetes: new test could detect the disease much earlier

Courtesy of Samuel Virtue, University of Cambridge
The glucose tolerance test is the standard method for detecting diabetes. But our new study suggests that a different test can identify the disease earlier than the glucose tolerance test.
Diabetes kills 3.4m people worldwide each year, and this figure is expected to continue rising. It kills people by causing secondary diseases, such as heart disease, stroke and kidney failure. And the longer diabetes remains untreated, the greater the risk of developing these diseases, so early detection is vital.
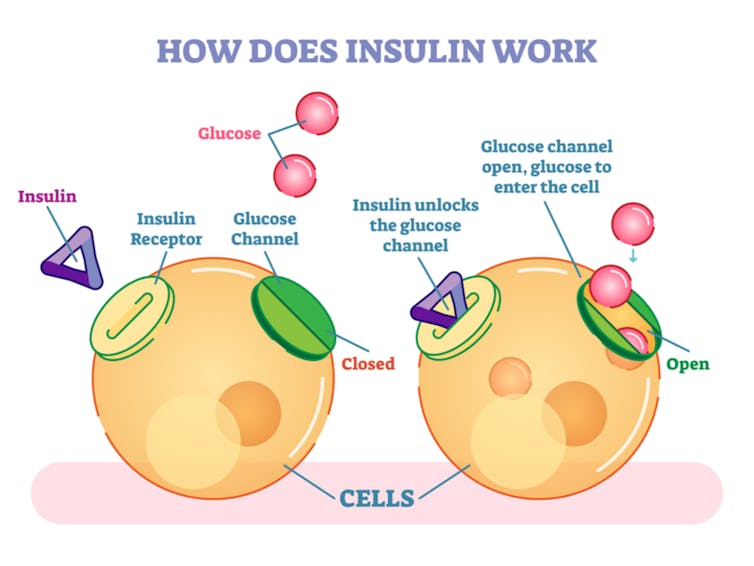
Diabetes is detected when the body can no longer regulate its own blood sugar levels. Blood sugar is controlled by insulin, a hormone made in the pancreas. This hormone lowers blood glucose by making the body’s cells take it up, where it is stored or used for energy.
There are two major forms of diabetes: type 1 and type 2. Type 1 is an autoimmune disease where the body destroys the cells in the pancreas that produce insulin. Type 2 is a progressive disease where the body first becomes resistant to insulin. Initially, the body makes more insulin to keep blood sugar levels in check, but the pancreas then wears out and blood glucose levels become dangerously high.
Fat as the new marker
In type 2 diabetes, the body’s cells become resistant to the effects of insulin before diabetes develops. This made us wonder whether we could detect earlier stages of the disease, when the body is insulin resistant but before the pancreas has worn out and blood glucose levels have increased. We focused on investigating how the body becomes unresponsive to insulin. And to do so, we considered fat, not glucose.
Obesity is now established as the leading cause of type 2 diabetes. One of the main ways that obesity is thought to cause diabetes is by the body fat (adipose tissue) not working properly.
Healthy adipose tissue takes up the fat we consume and stores it until it is needed for fuel, such as at night when we are asleep. When obese people eat a meal their adipose tissue does not take up the fat. Instead, the fat is directed into other organs, such as the liver and muscle where it causes insulin resistance.
Insulin acts as a signal and attaches to a receiver on the outside of cells called the insulin receptor. The insulin receptor activates lots of other signals inside the muscles or liver that tell them what to do, such as: take up glucose. But when the cell is full of fat, it muffles the signals, making them quieter. The fact the cells don’t respond to insulin makes them “insulin resistant”. The body tries to get around this by turning up the amount of insulin to make the cells take up the right amount of glucose, overcoming the effects of the fat.
Strong evidence
The concept that faulty adipose tissue can cause insulin resistance and diabetes is strongly supported by evidence from people with lipodystrophy – a condition where the body has no adipose tissue. People with this condition have severe insulin resistance and diabetes.
Importantly, the adipose tissue of obese people is also bad at releasing fat when they are asleep, meaning that obese people have to use lots of glucose when they are sleeping to provide energy.
The test doctors use to diagnose diabetes is called the glucose tolerance test. It is usually performed in the morning before people have eaten. The person is then given a drink containing glucose (sugar), and blood samples are taken over the next two hours.
People (and mice) are classed as having diabetes if they show high blood glucose levels during the test. But we suspected that some obese people would pass the test because their adipose tissue does not release enough fat and their body is primed to use glucose in fasted states, such as when they are asleep.
Conversely, if we gave obese people a large meal, the fat they should store in adipose tissue would go to organs, such as muscle, and cause insulin resistance, causing them to have high blood glucose.
Milkshake test
To study how fat causes insulin resistance and diabetes, we used mice lacking a gene called PPARy2. Removing the gene PPARy2 prevents adipose tissue from both taking up and releasing fat, mimicking what is seen in obese people.
Despite their fat not working properly, we already know that mice lacking PPARy2 appear healthy according to the glucose tolerance test. We now wanted to see if we could detect their defective fat using a large meal test. But there was a problem: how do you get a mouse to eat more food?
We exploited the fact that mice are normally fed a very boring diet, similar to rusks. When we switched mice to a tastier diet, high in fat, we realised they ate twice as much as normal for the first 24 hours after receiving the diet. We collected blood samples before and after the 24-hour overfeeding period to see if blood glucose and insulin increased.
We tested both normal mice and mice lacking PPARy2 with our overfeeding challenge. Normal mice increased their insulin levels twofold and kept their blood glucose levels normal. But mice lacking PPARy2 increased their insulin levels tenfold following the overfeeding challenge and had increased blood glucose levels, indicating that they were metabolically impaired.
Importantly, we conducted these tests in young mice, equivalent to people in their early twenties and at an age when their glucose tolerance tests were normal. Finally, we determined that when mice with defective adipose tissue reached middle age they became metabolically ill, even if they ate a healthy diet.
![]()
Our study suggests that it may be possible to detect some people with metabolic disease earlier by replacing the glucose in a glucose tolerance test with a calorific milkshake containing glucose, fat and protein. The next step will be to compare the ability of the glucose tolerance test and the milkshake test to predict future diabetes development in humans.
Samuel Virtue, Senior Research Associate, University of Cambridge
This article was originally published on The Conversation. Read the original article.



