Figuring out omicron – here’s what scientists are doing right now to understand the new coronavirus variant

A researcher works with COVID-19 samples from patients. Thomas Samson/AFP via Getty Images
Courtesy of Peter Kasson, University of Virginia
Scientists around the world have been racing to learn more about the new omicron strain of SARS-CoV-2, first declared a “variant of concern” on Nov. 26, 2021 by the World Health Organization. Officials cautioned that it would take several weeks before they’d know whether the recently emerged coronavirus variant is more contagious and causes more or less serious COVID-19 than delta and other earlier variants, and whether current vaccines can ward it off.
Peter Kasson is a virologist and biophysicist at the University of Virginia who studies how viruses such as SARS-CoV-2 enter cells and what can be done to stop them. Here he explains what lab-based scientists are doing to help answer the outstanding questions about omicron.
Does prior immunity protect against omicron?
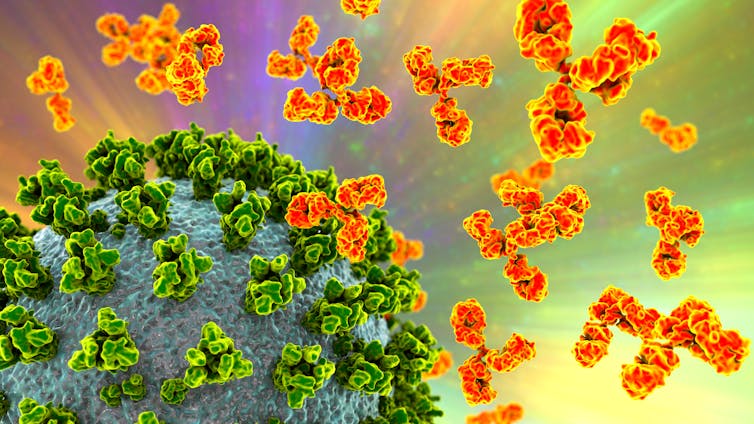
These are the key lab results everyone is waiting for: How effective are the antibodies people already have at fighting off omicron? If you got the booster shot, are you protected? Or if you had COVID-19 and then were vaccinated?
Will the antibodies people already have recognize and thwart omicron? Dr_Microbe/iStock via Getty Images
The goal is to see how well antibodies from real people who have had COVID-19 or have been vaccinated against it can hold off omicron in petri dishes in the lab. Scientists expect that antibodies from people exposed to other variants won’t work as well against omicron because of its mutations, but they need to measure how much less well and whether it’s still enough to stop the virus.
To answer these questions, most researchers first make a version of the SARS-CoV-2 virus that can enter cells but not reproduce. A few specialized labs with extra levels of biosecurity use the actual virus. Scientists add antibodies from the blood of people vaccinated against or recovered from COVID-19 to the virus. They then mix this with human lung cells to see whether the antibodies can stop the virus from infecting the cells.
My laboratory performs this kind of work with SARS-CoV-2 and other emerging viruses. Researchers have used these well-established techniques to test out antibodies after COVID-19 recovery, as well as different vaccines and different variants.
If antibodies people made against prior variants can’t stop omicron from infecting lung cells in the lab, then those antibodies probably won’t protect people out in the world either.
The very first early results are starting to come back, and it looks like antibodies against earlier variants are less successful at blocking omicron. Researchers took antibodies from six people who each had two doses of vaccine and from six other people who each had two doses of vaccine and had also recovered from an earlier COVID-19 infection. Antibodies from both groups of people were about 40 times worse at stopping omicron than original SARS-COV-2 strains, based on how much antibody was needed to prevent infection. But the people whose immune systems had seen the virus three times – that is, were doubly vaccinated and had also recovered from COVID-19 – had antibody levels that were high enough to still stop infection.
I’d expect people who have received booster vaccines will have similar or greater levels of immunity and will be at least moderately protected from omicron. But it will need to be tested. Pfizer has said their early results agree with this prediction, but the data is not yet publicly available. All of this work is not yet peer reviewed and still very preliminary.
Scientists will need to determine how a drop in “neutralization titer,” or how good antibodies are at blocking the virus in the lab, corresponds to a drop in “vaccine effectiveness” or how likely a vaccinated person is to get COVID-19 compared to an unvaccinated one. Scientists know that better antibodies correspond to more effective vaccines, but the precise numerical relationships need to be determined.

How contagious is omicron compared to delta?
The past pandemic year has shown that contagiousness, or transmissibility, has been the key factor in determining whether a coronavirus variant becomes dominant. Delta’s transmissibility has made it the current dominant variant because it simply outran others. But that situation may change with time.
The basic elements of the viral “life” cycle are getting into cells, making more virus, and getting out. Scientists can measure each of these stages in the lab and report what aspects of a variant make it more or less transmissible. In addition to binding to human cells better, some mutations enhance the packaging of new virus and the delivery of its genes once the virus gets into the cell.
While lab-based science can help people understand the biology behind just why a variant is more or less contagious, right now nature is doing a much bigger real-world experiment. Disease surveillance data from the U.K. and other countries where delta has been dominant suggest that omicron is gaining share and may eventually displace delta.
Exactly how this plays out may differ from one country to another, depending on factors like the number of vaccinated people and which variants were previously in circulation, but this news about how good omicron is at spreading is concerning.
Does omicron make people more or less sick?
This is again a question that will be answered much more quickly by the thousands of people infected with omicron than by work in the lab. It’s important to remember, though, that nature’s experiments are not as carefully controlled as lab experiments. Precise lab work will help explain why omicron might be different, but the first answers here will come from hospitals.
Lab-based scientists will be working with hospitals to analyze what makes some patients more or less sick once they contract omicron. Some early numbers suggest that the first omicron cases are mostly mild, but public health officials urge caution: Most cases of all COVID-19 variants are mild, and many of those infected so far with omicron are younger. Hospitalization counts tend to increase somewhat after the initial increase in cases. So this question will take time to answer.
Epidemiological data about how real patients are faring will fill in the picture. Apu Gomes/AFP via Getty Images
How are lab data and public health data complementary?
Laboratories will provide the first results on immune protection against omicron, although this will be followed up with public health data that will likely confirm the lab results. Public health data will bring the first results on contagiousness and disease severity, which will then be explained by laboratory results.
Once the initial answers from public health data are in, laboratory results are still important to understand why these changes happened and to help predict what future variants will do. How do officials declare a variant of concern in the first place? It’s a combination of public health data and understanding from the lab.
What do we know already?
Variants of SARS-CoV-2 don’t change the laws of physics and biology. They cannot leap tall buildings in a single bound. Physical barriers like high-grade masks and good ventilation will still stop the virus. And, very likely, vaccines will continue to provide some amount of protection. The question is how much, and whether the world needs to change the current vaccines or just provide more of them.
[Research into coronavirus and other news from science Subscribe to The Conversation’s new science newsletter.]![]()
Peter Kasson, Associate Professor of Molecular Physiology and Biomedical Engineering, University of Virginia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Chart: The Conversation, CC-BY-ND Source: CDC COVID Data Tracker Get the data Download image