How do viruses get into cells? Their infection tactics determine whether they can jump species or set off a pandemic
By Peter Kasson, University of Virginia
COVID-19, flu, mpox, noroviral diarrhea: How do the viruses that cause these diseases actually infect you?
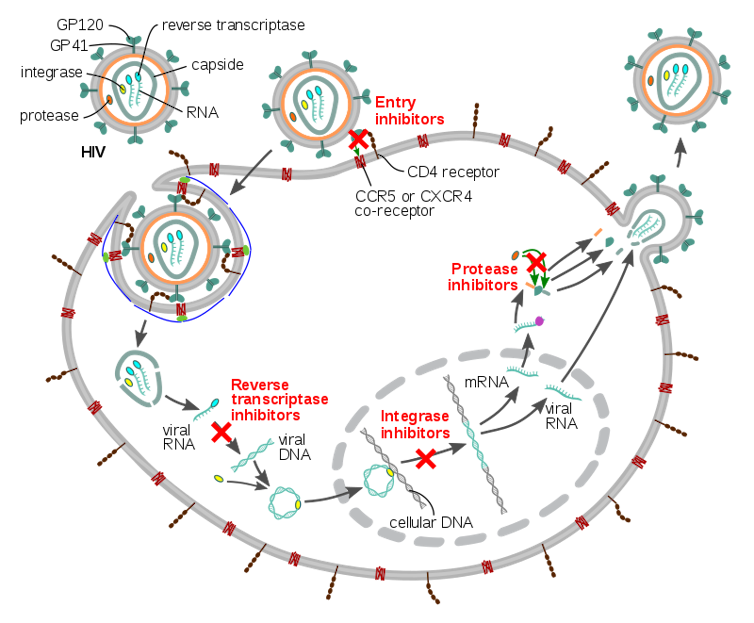
Viruses cannot replicate on their own, so they must infect cells in your body to make more copies of themselves. The life cycle of a virus can thus be roughly described as: get inside a cell, make more virus, get out, repeat.
Getting inside a cell, or viral entry, is the part of the cycle that most vaccines target, as well as a key barrier for viruses jumping from one species to another. My lab and many others study this process to better anticipate and combat emerging viruses.
How viruses enter cells
Different viruses travel into the body in various ways – via airborne droplets, on food, through contact with mucous membranes or through injection. They typically first infect host cells near their site of entry – the cells lining the respiratory tract for most airborne viruses – then either remain there or spread throughout the body.
Viruses recognize specific proteins or sugars on host cells and stick to them. Each virus gets only one shot at putting its genome inside a cell – if their entry machinery misfires, they risk becoming inactivated. So they use several mechanisms to prevent triggering entry prematurely.
After the virus binds to the cell, specific molecules on the cell’s surface or within the cell’s recycling machinery activate viral coat proteins for entry. An example is the SARS-CoV-2 spike that COVID-19 vaccines target. These proteins need to modify the cell membrane to allow the viral genome to get through without killing the cell in the process. Different viruses use different tricks for this, but most work like cellular secretion – how cells release materials into their environment – in reverse. Specialized viral proteins help merge the membranes of the virus and the cell together and release the viral core into the interior of the cell.
At this point, the viral genome can enter the cell and start replicating. Some viruses use only the cell’s machinery to replicate, while others carry along portions of their own replication machinery and borrow some parts from the cell. After replicating their genomes, viruses assemble the components required to make new viruses.
Two central questions scientists are studying about viral entry are how your body’s defenses can disrupt it and what determines whether a virus from other species can infect people.
Immune defenses against viruses
Your body has a multilayered defense system against viral threats. But the part of your immune system called the antibody response is generally thought to be most effective at sterilizing immunity – preventing an infection from taking hold in the first place as opposed to just limiting its scope and severity.
For many viruses, antibodies target the part of the virus that binds to cells. This is the case not just for current COVID-19 vaccines but also the majority of immunity against influenza, whether from vaccines or from prior infection.
However, some antibodies target the entry machinery instead: Rather than preventing the virus from sticking, they prevent the virus from working altogether. Such antibodies are often harder for the viruses to escape from but are difficult to reproduce with vaccines. For that reason, developing antibodies that inhibit cell entry has the been the goal of many next-generation vaccine efforts.
Species-hopping and pandemics
The other key question researchers are asking about viral entry is how to tell when a virus from another species poses a threat to people. This is particularly important because many viruses are first identified in animals such as bats, birds and pigs before they spread to humans, but it’s unclear which ones may cause a pandemic.
The part of viruses that stick to human cells varies the most across species, while the part that gets the virus into cells tends to stay mostly the same. Many researchers have thought that viruses changing in ways that bind better to human cells, like influenza viruses that bind to cells in the nose and throat, are some of the most important warning signs for pandemic risk.
However, coronaviruses – the family of viruses containing SARS-CoV-2 – are prompting re-examination of that idea. This is because several animal coronaviruses can actually bind to human cells, but only a few seem to be able to transmit well between people.
Only time will tell whether researchers need to broaden their pandemic prevention horizons or if their current prioritization of risky viruses is correct. The one grim reality of pandemic research, like earthquake research, is that there will always be another one – we just don’t know when or where, and we want to be ready.![]()
Peter Kasson, Professor of Molecular Physiology and Biomedical Engineering, University of Virginia
This article is republished from The Conversation under a Creative Commons license. Read the original article.